Or maybe that should be "non-interoperability"? Anyway, I have ranted in the past about the state of the EMR industry. I thought I'd add a little meat to the bone so you could better appreciate the hurdles facing device interoperability in healthcare today.
Here's a list of the standards and organizations that make up the many components of health information systems. I'm sure that I've missed a few, but these are the major ones:
Medical Coding
- SNOMED (Standardized Nomenclature for Medicine)
- LOINC (Logical Observation Identifiers Names and Codes)
- ICD9/10 (The International Classification of Diseases)
- CPT (Current Procedural Terminology)
Organizations
- FDA CDRH (Food and Drug Administration Center for Devices and Radiological Health)
- NHIH (National Health Information Network)
- HIMSS (Healthcare Information and Management Systems Society)
- CCHIT (Certification Commission for Healthcare Information Technology)
- PHIN (Public Health Information Network)
- VISTA (Veterans Health Information Systems and Technology Architecture)
Standards
- HL7 (Health Level Seven: v2 and v3)
- HIPAA (The Health Insurance Portability and Accountability Act of 1996)
- 21 CFR Part 11 (FDA/HHS Electronic Records and Signatures)
- IEEE-1073 (Point of Care Medical Device Communications)
- IHE (Integrating the Healthcare Enterprise)
- DICOM (Digital Imaging and Communications in Medicine)
- HITSP (Healthcare Information Technology Standards Panel)
- EHRVA (HIMSS Electronic Health Record Vendors' Association)
- NCPDP (National Council for Prescription Drug Programs)
- openEHR (International Foundation that promotes Electronic Health Records)
- CEN (European Committee for Standardization)
- CCR (Continuity of Care Record)
- ANSI X12 (Electronic Data Interchange)
- MLLP (Minimal Lower Layer Protocol)
- ebXML (Electronic Business using eXtensible Markup Language)
This list does not include any of the underlying transport or security protocols. They are either data formatting (many based on XML) or specialized messaging systems.
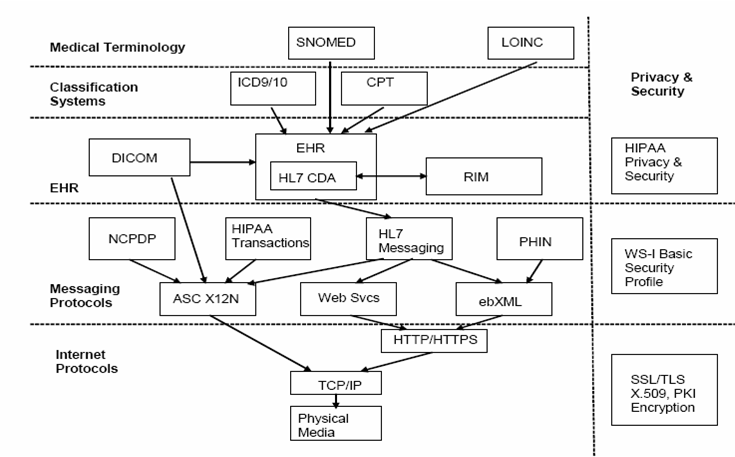
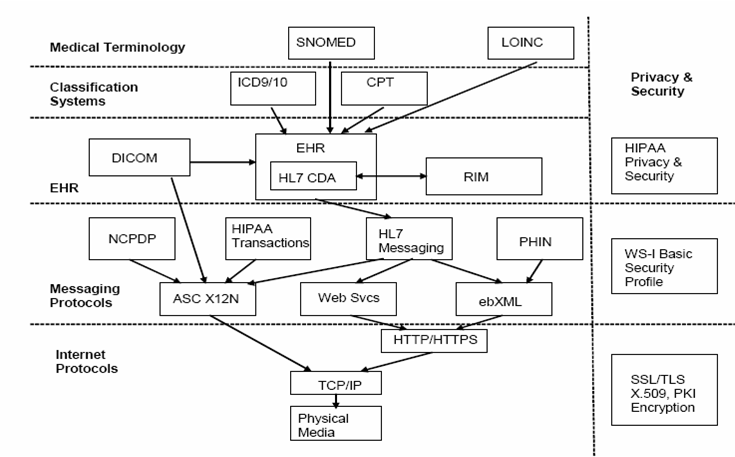
The diagram below gives an overview of how many of these standards are related (from an IEEE-USA purchased e-book -- copying granted for non-commercial purposes):
I don't know about you, but trying to make sense of all these standards and protocols is not an easy task. A discussion of next generation PHRs summarizes the situation well:
... not only is information scattered, but standards for defining and sharing the data are still evolving; where standards exist, many of them predate the Internet. Standards about how to define consistently the information (clinical standards) and to transmit and exchange the information (technical standards) are not yet formalized and agreed upon.
The point about predating the Internet is an important one. This particularly pertains to HL7 v2.x which still uses ASCII delimited messages for transmission over serial lines. For all you 21st century programmers that may have never seen one before, here's what an HL7 v2.x message looks like:
MSH|^~\&|AcmeHIS|StJohn|ADT|StJohn|20060307110111||ADT^A04
|MSGID20060307110111|P|2.4EVN|A04PID|||12001||Jones^John|
|19670824|M|||123 West St.^^Denver^CO^80020^USAPV1||O
|OP^PAREG^||||2342^Jones^Bob|||OP|||||||||2|||||||||||||||
||||||||||20060307110111|AL1|1||3123^Penicillin
||Produces hives~Rash~Loss of appetite
HL7 v3 uses XML for it's message format but it has not been widely adopted yet. A good history of HL7 v2 and v3, and an explanation of their differences, can be found here (pdf).
HL7 v2 is commonly used in hospitals to communicate between medical devices and EMR/HIS systems. Even though the communications framework is provided by HL7, new interfaces must still be negotiated, developed, and tested on a case-by-case basis.
Most of the large EMR companies provide HL7 interfaces, but many of the smaller ones do not. This is because hospitals are not their primary market so they don't generally need device interfaces. These EMRs are essentially clinical document management, patient workflow, and billing systems. The only external data they may deal with are scanned paper documents that can be attached to a patients record. The likelihood that they would conform to any of the standards listed above is low.
I'm not sure things will improve much with the recent PHR offerings from Microsoft (HealthVault) and Google (Google Health -- not yet launched) . Microsoft appears to be embracing some of these standards as discussed in Designing HealthVault’s Data Model, but there are a couple of telling comments:
Some of the data types we needed in order to support our partners’ applications where not readily available in the standards community.
Our types also allow each vendor to add “extensions” of their own making to item data – so to the extent that we are missing certain fields, they can be added – and the industry can rally around those extensions if it makes sense.
Microsoft says they are not the "domain experts", so they're leaving it to the industry to sort it all out. Great! This is probably the same attitude that got us to where we are today.
Hopefully you can now see why I've used the words "mess" and "chaos" to describe the current situation. The challenges facing interoperability in healthcare are immense.