I guess I've been obsessed with interoperability (or lack thereof) lately.
Definitions:
interoperability
Dictionary interoperability 1,0,0,0;interoperability=555039
- Main Entry: in·ter·op·er·a·bil·i·ty

- Pronunciation: \ˌin-tər-ˌä-p(ə-)rə-ˈbi-lə-tē\
- Function: noun
- Date: 1977
- : ability of a system (as a weapons system) to work with or use the parts or equipment of another system
Interoperability:
The ability of two or more systems or components to exchange information and to use the information that has been exchanged.
From the National Alliance for Health Information Technology (NAHIT) definition:
In healthcare, interoperability is the ability of different information technology systems and software applications to communicate, to exchange data accurately, effectively, and consistently, and to use the information that has been exchanged.
The four NAHIT levels are:
- Non-electronic data. Examples include paper, mail, and phone call.
- Machine transportable data. Examples include fax, email, and un-indexed documents.
- Machine organizable data (structured messages, unstructured content). Examples include HL7 messages and indexed (labeled) documents, images, and objects.
- Machine interpretable data (structured messages, standardized content). Examples include the automated transfer from an external lab of coded results into a provider’s EHR. Data can be transmitted (or accessed without transmission) by HIT systems without need for further semantic interpretation or translation.
From IEEE 1073 (Point of Care Medical Device Communications) and IEEE-USA Interoperability for the National Health Information Network (NHIN) -- original definitions are from IEEE Standard Computer Dictionary: Compilation of IEEE Standard Computer Glossaries, IEEE, 1990:
Functional: The capability to reliably exchange information without error.
- Shared architectures (conceptual design)
- Shared methods (processes and procedures)
- Shared frameworks (goals and strategies)
An architecture is the conceptual design of the system. Systems inter-operate if their architectures are similar enough that functions that execute on one system execute identically (or nearly identically) on another system.
Shared methods refer to the processes and procedures that a system performs. To ensure interoperability, these operations must be capable of being performed identically at any point in the network, regardless of implementation.
A shared framework is a shared set of goals and strategies. Stakeholders must agree on a shared set of goals and approaches to implementation.
Semantic: The ability to interpret, and, therefore, to make effective use of the information so exchanged.
- Shared data types (types of data exchanged)
- Shared terminologies (common vocabulary)
- Shared codings (standard encodings)
Shared data types refer to the types of data exchanged by systems. Interoperability requires that systems share data types on many different levels, including messaging formats (e.g. XML, ASCII), and programming languages (e.g. integer, string).
Shared terminologies refer to establishing a common vocabulary for the interchange of information. Standardized terminology is a critical requirement for healthcare applications to ensure accurate diagnosis and treatment, and has led to developing standards such as SNOMED-CT.
Shared codings refer to establishing standard encodings to be shared among systems. Codings refer not only to encoding software functions, but also to encoding medical diagnoses and procedures for claims processing purposes, research, and statistics gathering (e.g. ICD9/10, CPT).
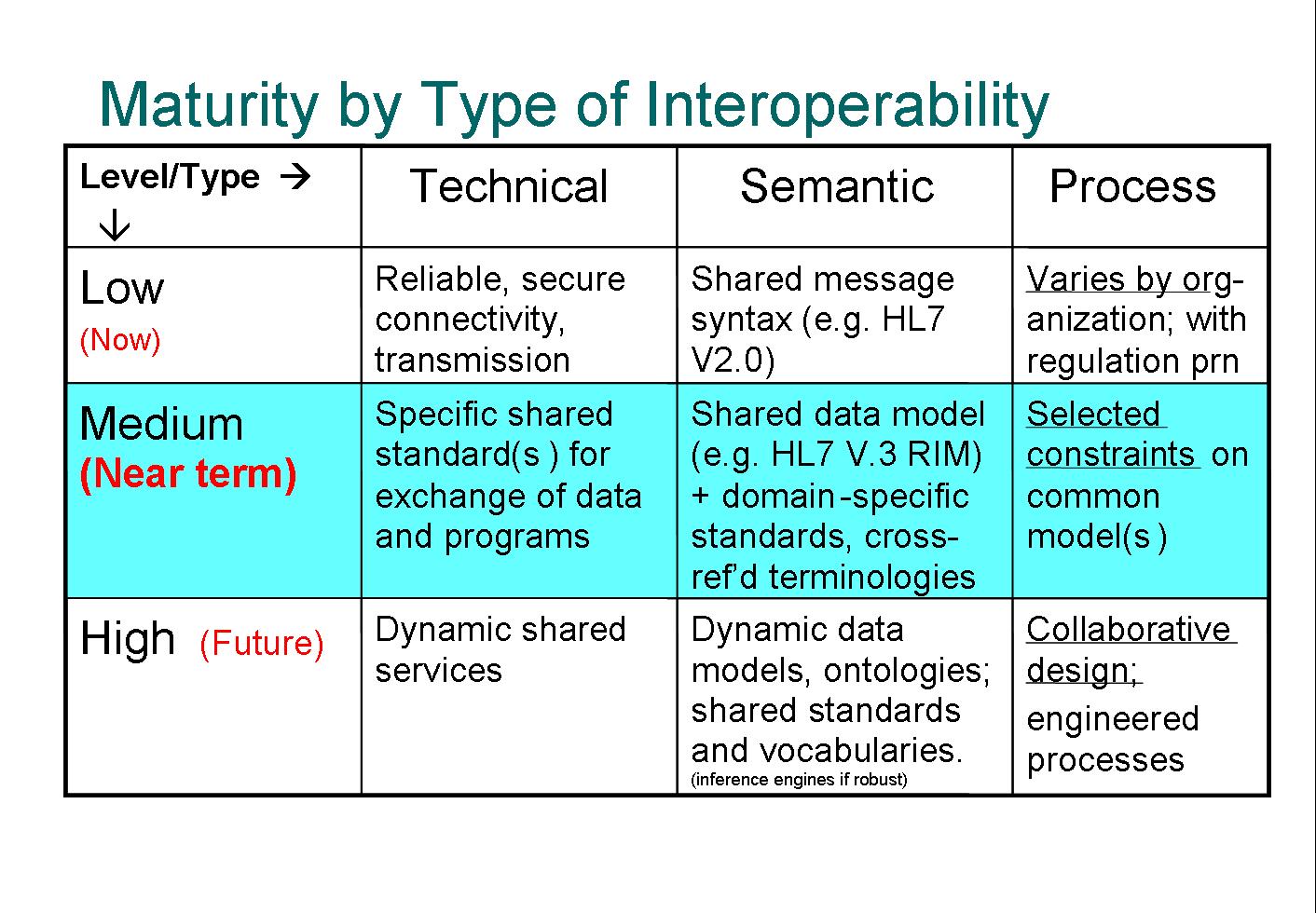
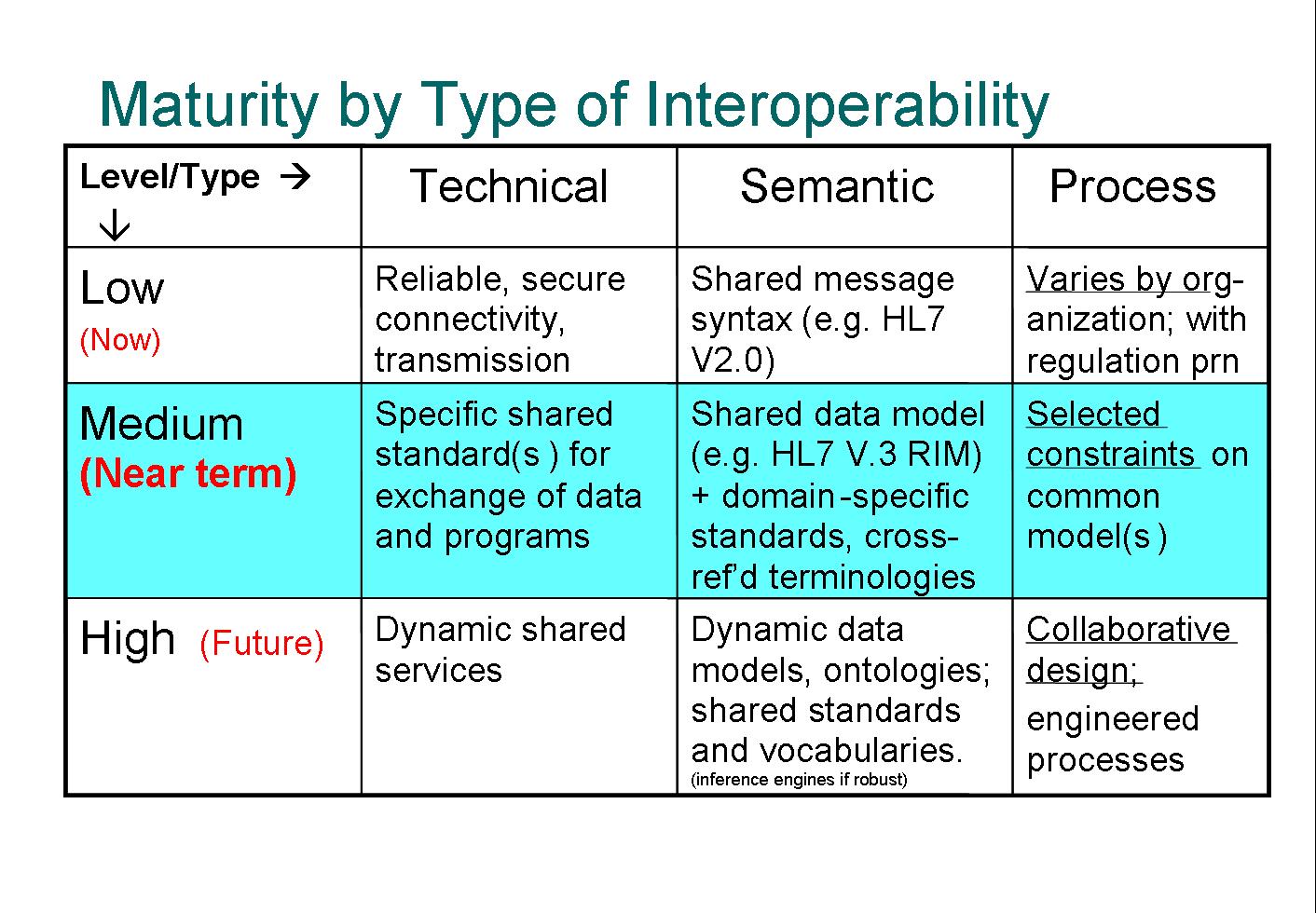
At Healthcare Informatics Technology Standards Panel (HITSP) I came across a maturity model of interoperability types from the Mayo Clinic. Even though this table is taken out of context, the Technical-Semantic-Process model shows yet another view of interoperability.
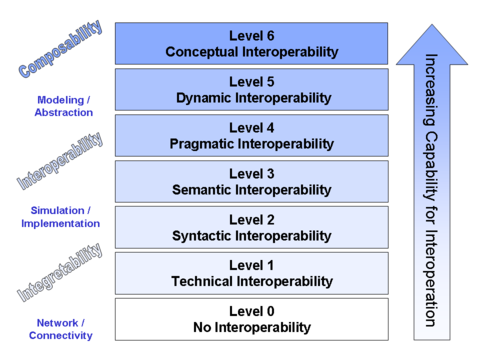
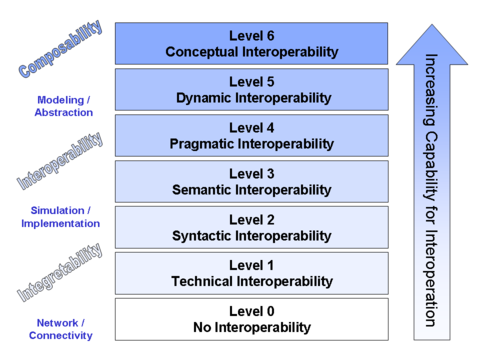
There are also a number of Models of Interoperability that describe abstract interoperability. For example, a finer grained layered model is called Conceptual Interoperability. This model encompasses the previous healthcare IT definitions:
Besides these definitions there are many articles (and books), especially as it relates to healthcare and EMR/EHR, that espouse the benefits of interoperability.
From a broader software industry point of view you can imagine the number and variety of issues that a company like Microsoft has to deal with. They claim Interoperability by Design. Of course Microsoft has gotten a lot of attention about their push to get Open Office XML (OOXML) approved as a standard by EMCA -- some quite negative:

Even though I don't believe the healthcare industry has the equivalent of 'Da Bill' (or maybe it does?), this points out one of the necessary components for the implementation of interoperability: standards.
I was on an ASTM standards committee a number of years ago (E1467-94, now superseded) , so I have some understanding of how difficult it is to get consensus on these types of issues. The process is long (years) and can sometimes be contentious. Even after a standard has been balloted and approved, there's no guarantee that it will be widely adopted.
Summary:
In my previous post on this subject I pointed out the plethora of healthcare IT standards and their confusing inter-relationships. The definitions of interoperability can be just as confusing. Each of the different models has a slightly different way of looking at the same thing. This is certainly one reason why there are so many overlapping standards.
Conculsion:
Interoperability in healthcare IT is multi-faceted and complex. This makes it difficult to agree upon exactly what it is (the definition) and even harder to develop the standards on which to base implementations.