This year's Medical Device Connectivity Conference is being held Sept. 28-29, 2010 in San Diego.
From the press release Tim Gee says:
The only conference devoted to the topic of medical device connectivity, the program will offer a unique opportunity to get immersed into every aspect of connectivity, workflow automation and enabling technologies. The keynotes and panel discussions on the first day frame the conference's focus on connectivity and tackle two of the biggest issues facing health care: industry standards and regulatory issues. Program tracks on the second day provide a survey of connectivity applications, clinical capabilities and outcomes, and explore the gap between regulated vendor-managed systems and the customer-managed and controlled environments in which these systems are used.
Here are just a few of the topics I'm particularly interested in:
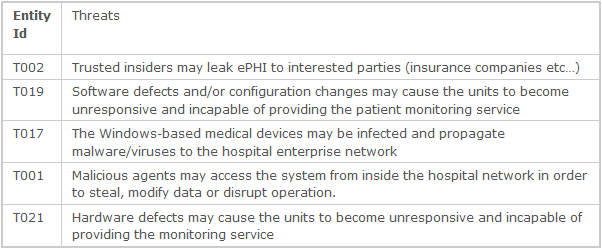
- EMERGING PROBLEMS AND RISING AWARENESS OF MEDICAL DEVICE SYSTEMS ON ENTERPRISE NETWORKS
- LOOKING BEYOND CONNECTIVITY IN HOSPITALS TO HOME HEALTH AND MOBILITY
- OPEN EHR MANIFESTSO: OPPORTUNITIES FOR MEDICAL DEVICE COMPANIES
- INTEROPERABLE MEDICAL DEVICE SYSTEM ARCHITECTURES
Looks like another great conference!


 There was a statement in one of the HIStalk
There was a statement in one of the HIStalk 